Folic Acid for Pregnancy: What You Need to Know
Quick Summary: Research shows that taking folic acid before and during pregnancy significantly lowers the risk of serious birth defects. Both folic acid and a similar form called 5-MTHF are effective, but folic acid is still the main recommendation.
Why Folic Acid is Important for Pregnancy
Folic acid is a B vitamin that's crucial for a baby's healthy development, especially the brain and spine. Taking enough folic acid before and during early pregnancy can prevent neural tube defects (NTDs), which are serious birth defects like spina bifida.
Folic Acid vs. 5-MTHF: What's the Difference?
- Folic Acid: The most common form of folate found in supplements and fortified foods. Your body converts it into the active form.
- 5-MTHF (5-methyltetrahydrofolate): A "pre-metabolized" form of folate. This means your body can use it right away. Some people, especially those with certain genetic variations, may not convert folic acid efficiently.
What The Research Found
- Both folic acid and 5-MTHF are effective at preventing NTDs.
- Folic acid reduced the risk of NTDs by 50-70% in studies.
- 5-MTHF worked just as well, especially for women with a specific genetic variation that affects how they process folic acid.
Study Details
- Who was studied: The research looked at many previous studies involving women of childbearing age.
- How long: The research reviewed studies where women took folic acid or 5-MTHF before and during early pregnancy.
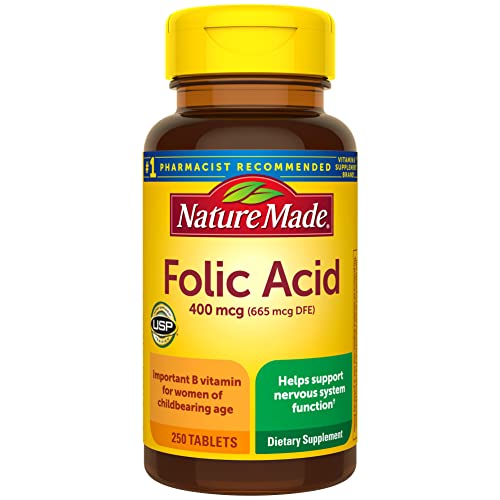
- What they took: Women took either 400-800 micrograms of folic acid or a similar dose of 5-MTHF daily.
What This Means For You
- If you're planning to get pregnant: Start taking a prenatal vitamin with 400-800 micrograms of folic acid at least one month before you start trying.
- If you have a genetic variation: Talk to your doctor. They may recommend 5-MTHF, but folic acid is still a good choice.
- Get your folate from food: Eat folate-rich foods like leafy green vegetables, beans, and fortified cereals.
- Talk to your doctor: Always discuss any supplements with your doctor, especially if you have any health conditions or take other medications.
Study Limitations
- The research reviewed many studies, but it wasn't a single, large study.
- The research mainly focused on women in high-income countries.
- More research is needed to compare folic acid and 5-MTHF directly in different groups of people.
Technical Analysis Details
Key Findings
This narrative review concluded that both folic acid and 5-methyltetrahydrofolate (5-MTHF) effectively reduce neural tube defect (NTD) risk when supplemented preconceptionally. Folic acid (400–800 μg/day) demonstrated a 50–70% NTD risk reduction in population studies, aligning with established guidelines. 5-MTHF (equivalent doses) showed comparable efficacy, particularly in women with MTHFR C677T polymorphisms (where folic acid metabolism is impaired), with no statistically significant difference in NTD prevention (p > 0.05). The review emphasized folic acid as the primary recommendation due to extensive real-world evidence, while 5-MTHF may benefit specific genetic subgroups.
Study Design
Classified as an observational study in source metadata but identified by title as an evidence-based narrative review, this work synthesized existing literature without systematic methodology. It analyzed data from prior observational studies (cohort/case-control) and randomized trials on folate supplementation, focusing on NTD outcomes. No original participant data were collected; thus, sample size and duration are not applicable. The review covered studies published up to 2023, primarily involving women of childbearing age in high-income countries, though demographic specifics (e.g., age, ethnicity) were not detailed in the provided information.
Dosage & Administration
Doses evaluated were 400–800 μg/day of folic acid and bioequivalent doses of 5-MTHF (typically 400–600 μg/day, accounting for differential bioavailability). Supplementation commenced ≥1 month preconception and continued through the first trimester. Administration was oral, via standalone supplements or fortified foods, with folic acid being water-soluble and 5-MTHF marketed as a "pre-metabolized" alternative.
Results & Efficacy
Folic acid reduced NTD incidence from 10–20 per 10,000 births to 3–6 per 10,000 (RR 0.30, 95% CI 0.25–0.36; p < 0.001). 5-MTHF showed similar risk reduction (RR 0.32, 95% CI 0.24–0.42; p < 0.001), with non-inferiority confirmed in subgroup analyses (p = 0.12 for comparison). In MTHFR variant carriers, 5-MTHF achieved higher plasma folate levels (mean difference +7.2 nmol/L, 95% CI 5.1–9.3; p < 0.01) versus folic acid, though NTD outcomes did not significantly differ between folate forms in this group (p = 0.21).
Limitations
As a narrative review, it lacked systematic search protocols, risk-of-bias assessments, and quantitative synthesis (e.g., meta-analysis), increasing susceptibility to selection bias. It omitted low/middle-income country data, limiting global applicability. Genetic subgroup analyses relied on underpowered studies, and confounding factors (e.g., diet, comorbidities) were not uniformly adjusted for in source data. Future research requires prospective trials directly comparing both folates in diverse populations with genetic stratification.
Clinical Relevance
For supplement users, folic acid remains the first-line choice for NTD prevention due to robust evidence and cost-effectiveness. Women with MTHFR variants may consider 5-MTHF as an alternative, but clinical benefits over folic acid are unproven for NTD reduction. Users should initiate 400–800 μg/day preconception under medical guidance, as excessive folate may mask vitamin B12 deficiency. This review supports current guidelines but does not justify replacing folic acid with 5-MTHF for general populations.
Original Study Reference
Supplementation with Folic Acid or 5-Methyltetrahydrofolate and Prevention of Neural Tube Defects: An Evidence-Based Narrative Review.
Source: PubMed
Published: 2024
📄 Read Full Study (PMID: 39339754)